View this short video clip in which Jill Bolte Taylor a research neuroscientist describes an opportunity few brain scientists would wish for: She had a massive stroke, and watched as her brain functions -- motion, speech, self-awareness -- shut down one by one. An astonishing story: www.ted.com/talks/jill_bolte_taylor_s_powerful_stroke_of_insight.html
The newly developed HandTutor and its sister devices (ArmTutor, LegTutor, 3DTutor) have become a key system in neuromuscular rehabilitation and physical therapy following strokes as well as other disabling diseases. These innovative devices implement an impairment based program with augmented feedback and encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient's performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient's ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation. See www.handtutor.com
Motor learning research evidence to support the HandTutor system, glove and dedicated rehabilitation software, method of and Physical and Occupational Therapy training for arm and hand functional ability improvement.
Monday 31 October 2011
How the Tutors Can Aid in Stroke Rehabilitation
Current statistics provided by the National Stroke Association indicate that there are over 4 million people in the United States who have survived a stroke or brain attack and are living with the after-effects. These numbers do not reflect the scope of the problem and do not count the millions of husbands, wives and children who live with and care for stroke survivors and who are, because of their own altered lifestyle, greatly affected by stroke.
The very word “stroke” indicates that no one is ever prepared for this sudden, often catastrophic event. Stroke survivors and their families can find workable solutions to most difficult situations by approaching every problem with patience, ingenuity, perseverance and creativity.
There’s still so much we don’t know about how the brain compensates for the damage caused by stroke or brain attack. Some brain cells may be only temporarily damaged, not killed, and may resume functioning. In some cases, the brain can reorganize its own functioning. Sometimes, a region of the brain “takes over” for a region damaged by the stroke. Stroke survivors sometimes experience remarkable and unanticipated recoveries that can’t be explained. General recovery guidelines show:
10 percent of stroke survivors recover almost completely
25 percent recover with minor impairments
40 percent experience moderate to severe impairments requiring special care
10 percent require care in a nursing home or other long-term care facility
15 percent die shortly after the stroke
Rehabilitation actually starts in the hospital as soon as possible after the stroke. In patients who are stable, rehabilitation may begin within two days after the stroke has occurred, and should be continued as necessary after release from the hospital.
Depending on the severity of the stroke, rehabilitation options include:
A rehabilitation unit in the hospital
A subacute care unit
A rehabilitation hospital
Home therapy
Home with outpatient therapy
A long-term care facility that provides therapy and skilled nursing care
The goal in rehabilitation is to improve function so that the stroke survivor can become as independent as possible. This must be accomplished in a way that preserves dignity and motivates the survivor to relearn basic skills that the stroke may have taken away – skills like eating, dressing and walking.
Improving functional capability of the stroke patient is the main goal of the Tutor system. Consisting of the HandTutor, ArmTutor, LegTutor and 3DTutor these newly developed devices optimize motor, sensory and cognitive performance to allow the patient to better perform everyday functional tasks and improve quality of life.
These innovative devices implement an impairment based program with augmented feedback and encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient’s performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient’s ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation. See www.handtutor.com
Complex Regional Pain Syndrome Therapy Includes the Tutor System

Prof. Dr. F. Birklein of the
Neurologische Klinik
Universität Mainz describes
Abstract Complex regional pain.
This syndrome (CRPS) may develop after limb trauma and is characterized by pain, sensory-motor and
autonomic symptoms. Most important for the understanding of the
pathophysiology of CRPS are recent results of neurophysiological
research. Major mechanism for
CRPS symptoms, which might be
present subsequently or in parallel
during the course of CRPS, are
trauma-related cytokine release,
exaggerated neurogenic inflammation, sympathetically maintained
pain and cortical reorganisation in
response to chronic pain (neuroplasticity). The recognition of these
mechanisms in individual CRPS
patients is the prerequisite for a
mechanism-oriented treatment.
In the beginning of the twentieth century, Paul Sudeck,
a surgeon in Hamburg, Germany, first published a paper
about post traumatic bone dystrophy [56]. He described
a posttraumatic pain syndrome with edema and trophic
changes.As the sympathetic nervous system seems to be
overactive at first glance, the term “Sympathetic Reflex
Dystrophy” was used for many years [11]. Studies, which
raised doubts on the role of the sympathetic nervous
system in the pathophysiology of this pain syndrome,
led to a new descriptive term – “Complex Regional Pain
Syndrome” (CRPS), the official one in recent years [55].
Treatment
The aims of CRPS therapy are the relief of pain and the
maintenance or restitution of function. To achieve this,
therapy has to start as soon as possible. One of the latest tools to be developed in the treatment of CRPS is the Tutor system. Consisting of the HandTutor, ArmTutor, LegTutor and 3DTutor these devices can speed the recovery and relieve the pain of the affected area
Image by Joe Shlabotnik via Flickr
.
The Tutor system has been developed to allow for functional rehabilitation of the whole body including the upper and lower extremity. The system consists of ergonomic wearable devices and dedicated rehabilitation software that provide patient instructions and feedback to encourage intensive massed controlled exercise practice. The Tutor system allows for controlled exercise of multijoints within the normal movement pattern which prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks. Additional features of the Tutor system include quantitative evaluation, objective follow up and tele-rehabilitation.
The new medical devices are available for children as well as adults and through the use of telerehabilitation and are FDA and CE certified. See www.handtutor.com
Tutor System Speeds Recovery for Brachial Plexus Injuries

BRACHIAL PLEXUS INJURIES
Upon initial evaluation of each patient it is important to begin the process noting previous studies, assessments made by Brachial Plexus physicians and any additional co-morbidities such as Torticollis, Diaphragmatic paralysis, Horner’s Syndrome, or clavicular fractures that may affect the treatment of these patients.
The physical evaluation then proceeds with the assessment of each patients function, active and passive range of motion. Different motor grading systems are available, however in our center the British Medical Research Council Muscle Grading system is utilized for the perinatal period in addition to the Mallet Classification in older children >2 years old.
Joint integrity in the glenohumeral, elbow, and wrist joints is evaluated and the presence of any malalignment is then noted. Clavicular and humeral fractures are ruled out. However, if present treatment in the form of joint protection and positioning are utilized. These fractures heal rapidly if recognized early.
Assessment of muscle tone is also made, observing for atrophy and normal development. A determination is made if the affected extremity is flaccid or hypotonic. A natural progression of tone will begin proximal to distal as nerve regeneration occurs. Age appropriate reflexes such as Moro, 3 months, and palmar grasp, 6 months, are utilized to assess the degree of injury and follow recovery. These reflexes will be absent in the affected arm and will be present with eventual recovery.
Sensations to sharp and dull pain, deep pressure, light touch, vibratory and proprioception are used to evaluate the level of injury. Sensation to pain may be difficult in the newborn period. However, facial grimaces, crying or protective reactions may help in our assessments or input from parents is always valuable. Noting the degree of awareness each child has for the affected extremity is also valuable as we have seen that patients with no awareness of the affected arm tend to have more severe injuries and slower recovery.
A final area of assessment is whether each patient is meeting developmental milestones through their growth. Gross motor and fine motor coordination are followed for age appropriate development. Social interactions with family, friends, teachers, in addition to relationships are assessed for proper development. Language and cognitive skills are also followed to ensure that each patient is at their age appropriate level.
The HandTutor and ArmTutor have been designed to achieve maximum range of motion and joint integrity to the wrist, elbow and arm of a patient recovering from a Brachial Plexus injury. The Tutor system can boost gross and fine motor coordination of the affected arm or shoulder.
The devices which include the LegTutor and 3DTutor have become a key system in neuromuscular rehabilitation and physical therapy. These innovative devices implement an impairment based program with augmented feedback and encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient’s performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient’s ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation.
Sunday 30 October 2011
Children With Brain Injury Benefit From Tutor System

Drs. JA Langlois ,W.Rutland-Brown etal of the Centers for Disease Control and Prevention and National Center for Injury Prevention and Control writing about a
population-based comparison of clinical and outcome characteristics of young children with serious inflicted and noninflicted traumatic brain injury.
Traumatic brain injury (TBI) is the leading cause of disability and death in children and adolescents in the U.S. According to the Centers for Disease Control and Prevention The two age groups at greatest risk for TBI are age 0-4 and 15-19.
Among those ages 0 to 19, each year an average of: 62,000 children sustain brain injuries requiring hospitalization as a result of motor vehicle crashes, falls, sports injuries, physical abuse and other causes
564,000 children are seen in hospital emergency departments for TBI and released.
Among children ages 0 to 14 years, TBI results in an estimated in:
2,685 deaths
37,000 hospitalizations
435,000 emergency department visits
In a report to Congress, Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths, the Centers for Disease Control and Prevention notes falls are the leading cause of TBI for children age 0-4. Approximately 1,300 U.S. children experience severe or fatal head trauma from child abuse every year.
Any impairments may occur to different degrees. The nature of the injury and its consequences can range from mild to severe, and the course of recovery is very difficult to predict for any given child. With early diagnosis and ongoing therapeutic intervention, the severity of these symptoms may decrease in varying degrees. Symptoms can vary greatly depending on the extent and location of the brain injury. Impairments in one or more areas (such as cognitive functioning, physical abilities, communication, or social/behavioral disruption) are common.
What makes a brain injury in children different?
While the symptoms of a brain injury in children are similar to the symptoms experienced by adults, the functional impact can be very different. Children are not little adults. The brain of a child is continuing to develop. The assumption used to be a child with a brain injury would recover better than an adult because there was more “plasticity” in a younger brain. More recent research has shown that this is not the case. A brain injury actually has a more devastating impact on a child than an injury of the same severity has on a mature adult. The cognitive impairments of children may not be immediately obvious after the injury but may become apparent as the child gets older and faces increased cognitive and social expectations for new learning and more complex, socially appropriate behavior. These delayed effects can create lifetime challenges for living and learning for children, their families, schools and communities. Some children may have lifelong physical challenges. However, the greatest challenges many children with brain injury face are changes in their abilities to think and learn and to develop socially appropriate behaviors.
Common deficits after brain injury include difficulty in processing information, impaired judgment and reasoning. When an adult is injured, these deficits can become apparent in the months following the injury. For a child, it may be years before the deficits from the injury become apparent. An example of this is described in the story of “Betsy.”
Betsy was an active, inquisitive 6 year old girl. She was involved in a motor vehicle accident and sustained a moderate brain injury. She was treated at the hospital and discharged to home with outpatient therapies to continue her recovery. She missed a little over a month of school as she recovered. She was able to return to her first grade class, and with help from teachers and her parents, was able to complete the school year with average grades. She needed help in learning new things, but was able to remember them with extra repetitions.
Betsy continued in school, getting average or above average grades. It wasn’t until she reached fifth grade that her grades started to decline. Teachers and her parents did not understand the change. She went to school, she tried to do her homework every night. She complained that she just didn’t understand the schoolwork anymore. She became more irritable and argued with the teachers at times. No one thought to connect the brain injury years ago with her current issues.
Betsy was experiencing the long term effects of brain injury in children Her schoolwork increased in complexity, and required more sophisticated problem solving. The areas of the brain responsible for those functions were injured in the accident. Until now, those skills of abstract reasoning and more complex problem solving were not expected to be present. It was only when Betsy “grew into her injury” that her deficits became more readily apparent.
Fortunately, the mom was able to find her local Brain Injury Association and ask them about why Betsy was having trouble now. Information about the “neurocognitive stall”after a brain injury was sent to her, and she was connected with a professional that had experience working with children with brain injury. It will be a longer road to recover from her brain injury than anyone originally imagined, but Betsy, now connected with the right resources, has a much better chance of meeting the challenges of her brain injury.
When children with TBI return to school, their educational and emotional needs are often very different than before the injury. Their disability has happened suddenly and traumatically. They can often remember how they were before the brain injury. This can bring on many emotional and social changes. The child’s family, friends and teachers also recall what the child was like before the injury and may have adjusting their expectations of the child.
It is extremely important to plan carefully for the child’s return to school. Parents will want to find out ahead of time about special education services offered in their community. This information is usually available from the school’s principal or special education teacher. The school will need to evaluate the child thoroughly. This evaluation will let the school and parents know what the student’s educational needs are. The school and parents will then develop an Individualized Education Program (IEP) that addresses those educational needs.
Remember the IEP is a flexible plan. It can be changed as the parents, the school and the student learn more about what the student needs at school.
Learn about TBI. The more you know, the more you can help yourself and your child. See the list of resources and organizations below.
Work with the medical team to understand your child’s injury and treatment plan. Don’t be shy about asking questions. Tell them what you know or think. Make suggestions.
Keep track of your child’s treatment. A 3-ring binder or a box can help you store this history. As your child recovers, you may meet with many doctors, nurses and others. Write down what they say. Put any paperwork they give you in the notebook or keep it in the box. If you are asked to share your paperwork with someone else, make a copy. Don’t give away your original.
Talk to other parents whose children have sustained a brain injury. There are parent groups all over the U.S. Parents can share practical advice and emotional support. Check with your local Brain Injury Association to find parent groups near you.
College or any type of post secondary education for people with brain injury used to be considered an “unrealistic expectation” of life after brain injury. However, there are more students with brain injury investigating and attending college. The Brain Injury Association’s National Brain Injury Information Center notes that inquiries about college options for students with brain injuries has significantly increased over the last decade. There are now a range of resources available to families to help them work through the decision making process.
Concussion in children is common. Parents often ask, “When it is safe for a child to return to play or other activities?” and “How can I help my child recover from a concussion?”
Infants, Toddlers and Preschool Children
Very young children (i.e. infants, toddlers, and preschoolers) frequently sustain bumps and bruises to their heads from a host of mechanisms including falls (down stairs or from heights such as counter tops or beds), direct impacts (e.g. getting hit in the head with a ball), motor vehicle crashes, tricycle/bike accidents or child abuse.
Sometimes these events can be significant enough to result in a concussion. Deciding whether a child who has hit his or her head needs an immediate concussion assessment can be difficult. Young children may have the same concussion symptoms as older children, but they do not express them in the same way. For example, young children cannot explain a feeling of nausea or amnesia or even describe where they hurt. Parents and physicians should keep this in mind when considring the presence of concussion symptoms listed below. When in doubt, refer a child for immediate evaluation. Primary care physicians (PCPs) should ask caregivers about all “bumps on the head” and should consider referring a child with a “bump on the head” to the emergency department if they suspect a concussion.
Young children may also sustain mild to severe TBIs from abuse.
Approximately 1,400 cases of abusive TBI (including concussions) occur in the U.S. each year.
Injuries resulting from abusive TBI and other types of child maltreatment are often unrecognized or underreported.
Recognition of abusive TBI in young children is critical. If children are returned to a violent home, they are at very high risk of being hurt again or killed.
In any young child with injury to the head, it is imperative to assess whether the history provided for the injury is developmentally appropriate for a child that age. If not, it is important to consider child abuse in the differential diagnosis.
In some cases of abuse, caretakers do not report a history of any trauma either because (a) they do not know that there has been trauma because it is being inflicted by someone else without their knowledge or (b) because they don’t want to tell. As a result, if an infant or young child presents with the signs and symptoms listed above, it is important to consider the possibility of abusive TBI even in the absence of a history of trauma.
Seizures
Dizziness or confusion
Change in personality
Change in nursing or eating habits
Becoming upset easily or increased temper tantrums
Sad or lethargic mood
Lack of interest in favorite toys
Source: Centers for Disease Control and Prevention’s Toolkit for Physicians
To reduce the risk of sustaining a TBI, individuals should:
Wear a seat belt every time they drive or ride in a motor vehicle.
Buckle children the car using a child safety seat, booster seat, or seat belt according to the child’s height, weight and age. Children should start using a booster seat when they outgrow their child safety seats, usually when they weigh about 40 pounds. Children should continue to ride in a booster seat until the lap/shoulder belts in the car fit properly, typically when they are approximately 4’9″ tall.
Wear a helmet and make sure children wear helmets that are fitted properly.
Make sure playground surfaces are made of shock-absorbing materials, such as hardwood mulch or sand, and are maintained to an appropriate depth.
Use the right protective equipment and make sure it is maintained properly.
Make living areas safer for children by:
Installing window guards to keep young children from falling out of open windows;
Using safety gates at the top and bottom of stairs when young children are around;
Keeping stairs clear of clutter;
Securing rugs and using rubber mats in bathtubs; and
Not allowing children to play on fire escapes or on other unsafe platforms.
Make sure playground surfaces are made of shock-absorbing materials, such as hardwood mulch or sand, and are maintained to an appropriate depth.
The newly developed Tutor system has been designed for children as well as adults who suffer from brain injury.
The Tutor system, consisting of the HandTutor, ArmTutor, LegTutor and 3DTutor, has been developed to allow for functional rehabilitation of the whole body including the upper and lower extremity. The system consists of ergonomic wearable devices and dedicated rehabilitation software that provide patient instructions and feedback to encourage intensive massed controlled exercise practice. The Tutor system allows for controlled exercise of multijoints within the normal movement pattern which prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks. Additional features of the Tutor system include quantitative evaluation, objective follow up and tele-rehabilitation.
The new medical devices are available through the use of telerehabilitation and are FDA and CE certified.
Cognitive Impairments Treated by Tutor System

The Committee on Cognitive Rehabilitation Therapy for Traumatic Brain Injury, in reference to a report released by the Institute of Medicine (IOM) on Oct. 11, 2011“Cognitive Rehabilitation Therapy for Traumatic Brain Injury: Evaluating the Evidence,” said “There is some evidence about the potential value of cognitive rehabilitation therapy (CRT) for treating traumatic brain injury (TBI), but overall it is not sufficient to develop definitive guidelines on how to apply these therapies and to determine which type of CRT will work best for a particular patient.” BIAA agrees with IOM’s findings and supports the call for additional research to demonstrate the therapeutic effectiveness of different interventions in improving cognition after brain injury.
The Committee on Cognitive Rehabilitation Therapy, which is comprised of representatives from the National Academy of Sciences, the National Academy of Engineering, the Institute of Medicine and the National Research Council, supports the ongoing use of CRT for people with TBI while improvements are made in the standardization, design and conduct of studies.
BIAA, in cooperation with the Wounded Warrior Project (WWP), was the force behind authorizing this study in the FY2009 National Defense Authorization Act. BIAA acknowledges the need for additional research, further development of clinical guidelines and modification to public systems of care and private sector insurance policies. In the meantime, BIAA and WWP are committed to finding ways for injured service members to access cognitive rehabilitation techniques by enjoying an open dialogue with Dr. Warren Lockette, chief medical officer of TRICARE Management Activity.
The newly developed Tutor system consisting of the HandTutor, ArmTutor, LegTutor and 3DTutor has many benefits including the fact that it treats motor, sensory and cognitive impairments.
The Tutor system has become a key system in neuromuscular rehabilitation and physical therapy. The devices are used in physiotherapy not only for brain injury but also for victims of Parkinson’s, MS, CP, stroke, SPI, Radial and Ulnar nerve injuries, development and co-ordination disorders, Brachial Plexus injuries and other disabling diseases. These innovative devices implement an impairment based program with augmented feedback and encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient’s performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient’s ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation.
Living With Brain Injury and the Advantage of the Tutor System

Brain injury is unpredictable in its consequences. Brain injury affects who we are, the way we think, act, and feel. It can change everything about us in a matter of seconds. The most important things to remember:
• A person with a brain injury is a person first
• No two brain injuries are exactly the same
• The effects of a brain injury are complex and vary greatly from person to person
• The effects of a brain injury depend on such factors as cause, location, and severity
1.7 million people sustain a traumatic brain injury (TBI) each year. According to the Centers for Disease Control and Injury Prevention, the leading causes of TBI are:
• Falls (35.2%)
• Motor vehicle-traffic crashes (17.3%)
• Struck by/against events (16.5%)
• Assaults (10%)
A Healthy Brain
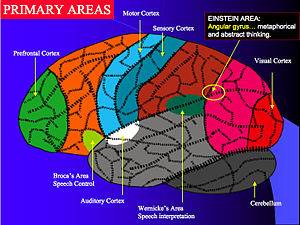
To understand what happens when the brain is injured, it is important to realize what a healthy brain is made of and what it does. The brain is enclosed inside the skull. The skull acts as a protective covering for the soft brain. The brain is made of neurons (nerve cells). The neurons form tracts that route throughout the brain. These nerve tracts carry messages to various parts of the brain. The brain uses these messages to perform functions. The functions include our coordinating our body’s systems, such as breathing, heart rate, body temperature, and metabolism; thought processing; body movements; personality; behavior; and the senses, such as vision, hearing, taste, smell, and touch. Each part of the brain serves a specific function and links with other parts of the brain to form more complex functions. All parts of the brain need to be working well in order for the brain to work well. Even “minor” or “mild” injuries to the brain can significantly disrupt the brain’s ability to function.
An Injured Brain
When a brain injury occurs, the functions of the neurons, nerve tracts, or sections of the brain can be affected. If the neurons and nerve tracts are affected, they can be unable or have difficulty carrying the messages that tell the brain what to do. This can change the way a person thinks, acts, feels, and moves the body. Brain injury can also change the complex internal functions of the body, such as regulating body temperature; blood pressure; bowel and bladder control. These changes can be temporary or permanent. They may cause impairment or a complete inability to perform a function.
Functions of the Brain
The brain is divided into main functional sections, called lobes. These sections or brain lobes are called the Frontal Lobe, Temporal Lobe, Parietal Lobe, Occipital Lobe, the Cerebellum, and the Brain Stem. Each has a specific function as described below.
Parietal Lobe Functions
Sense of touch
Spatial perception
Differentiation (identification) of size, shapes, and colors
Visual perception
Occipital Lobe Functions
Vision
Cerebellum Lobe Functions
Balance
Skilled motor activity
Coordination
Visual perception
Brain Stem Functions
Breathing
Arousal and consciousness
Attention and concentration
Heart rate
Sleep and wake cycles
Frontal Lobe Functions
Attention and concentration
Self-monitoring
Organization
Speaking (expressive language)
Motor planning and initiation
Awareness of abilities and limitations
Personality
Mental flexibility
Inhibition of behavior
Emotions
Problem solving
Planning and anticipation
Judgment
Temporal Lobe Functions
Memory
Understanding language (receptive language)
Sequencing
Hearing
Organization
Right or Left Brain
The functional sections or lobes of the brain are also divided into right and left sides. The right side and the left side of the brain are responsible for different functions. General patterns of dysfunction can occur if an injury is on the right or left side of the brain.
Injuries of the left side of the brain can cause:
Difficulties in understanding language (receptive language)
Difficulties in speaking or verbal output (expressive language)
Catastrophic reactions (depression, anxiety)
Verbal memory deficits
Impaired logic
Sequencing difficulties
Decreased control over right-sided body movements
Injuries of the right side of the brain can cause:
Visual-spatial impairment
Visual memory deficits
Left neglect (inattention to the left side of the body)
Decreased awareness of deficits
Altered creativity and music perception
Loss of “the big picture” type of thinking
Decreased control over left-sided body movements
Diffuse Brain Injury (The injuries are scattered throughout both sides of the brain) can cause:
Reduced thinking speed
Confusion
Reduced attention and concentration
Fatigue
Impaired cognitive (thinking) skills in all areas
When the brain injury causes impaired movement of upper or lower limbs the Tutor system has demonstrated remarkable improvement when integrated into the post stroke physiotherapy program.
Intensive exercise practice has shown to improve functional movement ability following orthopedic and neurological injury and disease. Patient motivation and control of the exercise practice are the fundamental factors that are required for optimum functional recovery. Traditional practice is mostly based on low technology tools that intrinsically lack features to challenge and motivate the patient to intensive exercise training. In addition low technology tools do not provide sufficient resolution to completely control the required exercise performance.
The Tutor system, consisting of the HandTutor, ArmTutor, LegTutor and 3DTutor, has been developed to allow for functional rehabilitation of the whole body including the upper and lower extremity. The system consists of ergonomic wearable devices and dedicated rehabilitation software that provide patient instructions and feedback to encourage intensive massed controlled exercise practice. The Tutor system allows for controlled exercise of multijoints within the normal movement pattern which prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks. Additional features of the Tutor system include quantitative evaluation, objective follow up and tele-rehabilitation.
Currently in use in leading U.S. and foreign hospitals and clinics the new medical devices are available for children as well as adults and through the use of telerehabilitation and are FDA and CE certified.
Thursday 27 October 2011
Treating Stroke Includes the Tutor System in Rehabilitation

TREATING STROKE
Image via Wikipedia
What is good stroke care?
Effective treatment of stroke has been found to prevent long-term disability and save lives according to a National Institute of Health report.. The National Stroke Strategy was published in December 2007, and provides a guide to high quality health and social care for those affected by stroke. Stroke experts have set out standards which define good stroke care, including:
a rapid response to a 999 call for suspected stroke
prompt transfer to a hospital providing specialist care
an urgent brain scan (for example, computerised tomography [CT] or magnetic resonance imaging [MRI]) undertaken as soon as possible
immediate access to a high quality stroke unit
early multidisciplinary assessment, including swallowing screening
stroke specialised rehabilitation
planned transfer of care from hospital to community and longer term support
The National Institute for Health and Clinical Excellence (NICE) has produced a quality standard for stroke that describes the level of care that the NHS is working towards.
If you are concerned about the standard of care provided, speak to your stroke specialist or a member of the stroke team.
Ischaemic strokes
Ischaemic strokes can be treated using a ‘clot-busting’ medicine called alteplase, which dissolves blood clots (thrombolysis). However, alteplase is only effective if started during the first four and a half hours after the onset of the stroke. After that time, the medicine has not been shown to have beneficial effects. Even within this narrow time frame, the quicker alteplase can be started the better the chance of recovery. However, not all patients are suitable for thrombolysis treatment.
You will also be given a regular dose of aspirin (an anti-platelet medication), as this makes the cells in your blood, known as platelets, less sticky, reducing the chances of further blood clots occurring. If you are allergic to aspirin, other anti-platelet medicines are available.
Anticoagulants
You may also be given an additional medication called an anticoagulant. Like aspirin, anticoagulants prevent blood clots by changing the chemical composition of the blood in a way that prevents clots from occurring. Heparin and warfarin are two anticoagulants that are commonly used.
Anticoagulants are often prescribed for people who have an irregular heartbeat that can cause blood clots.
Blood pressure
If your blood pressure is too high, you may be given medicines to lower it. Two medicines that are commonly used are:
thiazide diuretic: this reduces the amount of water in your body and widens the blood vessels, which decreases blood pressure
angiotensin converting enzyme (ACE) inhibitors: these widen the blood vessels and reduce blood pressure
Statins
If the level of cholesterol in your blood is too high, you will be given a medicine known as a statin. Statins reduce the level of cholesterol in your blood by blocking an enzyme (chemical) in the liver that produces cholesterol.
Carotid stenosis
Some ischaemic strokes are caused by a narrowing in the carotid artery, which is an artery in the neck, which takes blood to the brain. The narrowing, known as carotid stenosis, is caused by a build-up of fatty plaques.
If the carotid stenosis is particularly bad, surgery may be used to unblock the artery. This is done using a surgical technique called a carotid endarterectomy. It involves the surgeon making an incision in your neck in order to open up the carotid artery and remove the fatty deposits.
Follow up rehabilitation
Rehabilitation following even partial recovery of stroke can bring back a positive approach to life. The Tutor system has shown amazing success in stroke rehabilitation.
The newly developed HandTutor and its sister devices (ArmTutor, LegTutor, 3DTutor) have become a key system in neuromuscular rehabilitation and physical therapy. The Tutors have been shown to be effective not only for stroke patients but also for those suffering from Pakinson’s disease, Brain Injuries, Spinal Cord Injuries, CP, MS, Radial and Ulnar nerve injuries, Brachial Plexus Injuries and a variety of upper and lower limb surgeries. These innovative devices implement an impairment based program with augmented feedback and encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient’s performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient’s ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation.
Want to know more?
The Stroke Association:go to making sense of medication
Even Nuclear Engineers Can Suffer From Strokes and Recover With the Help of the Tutor Sytem

As reported on October 25, 2011 by the CNN Wire Staff. The American researcher, who was stranded in the South Pole for weeks after suffering a stroke, is finally back on American soil., Renee-Nicole Douceur, 58, landed at Washington’s Dulles International Airport Monday evening.
In an exclusive interview with CNN affiliate WJLA, Douceur said “I am so glad to be home. It’s great to be here. It’s great to be back in America”. Tuesday Douceur will be at Johns Hopkins Hospital to undergo additional testing and determine a plan for rehabilitation. Monday she told WJLA her condition is improving but she still struggles with speech, vision and memory problems.
The researcher’s experience began on August 27 when she became ill while working at the National Science Foundation’s Amundsen-Scott research station in Antarctica., She was unable to leave the station to receive treatment because weather and storms prevent planes from landing during the region’s winter period. “While I was devastated that I had a stroke, it was like, oh, my God, it just stymied me … and I cried,” Douceur said. “I just didn’t know what to do and the doctors basically told me, just go back to my room,” she said in a recent interview.
Raytheon Polar Services, the company that runs the station for the NSF, told CNN that Douceur’s station has a well-trained medical staff that can provide all levels of treatment for employees. Elizabeth Cohen, the senior medical correspondent for CNN, said it wasn’t the lack of doctors that was the issue. It was the lack of equipment and a stroke expert. “In the United States, or New Zealand they would have stroke experts who would be able to do imaging and see where that stroke was and do rehab specifically designed for that particular location of the brain where the stroke occurred. But they don’t have that there” Cohen said. Cohen said Douceur did some basic rehab while at the station which includes relearning math. “This is a nuclear engineer who is having trouble with sixth-grade math” Cohen said.
After several weeks of waiting, a U.S. Air Force C-17 plane was able to evacuate Douceur who was taken to Christchurch, New Zealand for testing before being able to come home to the U.S.,
The Tutor system is a widely used newly developed set of devices (HandTutor, ArmTutor, LegTutor, 3DTutor) that are used extensively in post stroke rehabilitation., The Tutor system has become a key system in neuromuscular rehabilitation and physical therapy. These innovative devices implement an impairment based program with augmented feedback and encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient’s performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient’s ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation.
Early Rehabilitation Includes the Tutor System

Good advice from WEB MD.
How Atherosclerosis Causes 50% of Strokes
Having a stroke is one of the most frightening prospects of aging. Strokes can come on suddenly, stealing the use of an arm or the ability to speak. A stroke can be fatal or leave us permanently disabled. About half of all strokes are caused by atherosclerosis — the same process of narrowing and hardening of the arteries that causes heart attacks. Atherosclerosis progresses silently, without symptoms, putting our brains and our independence at risk.
Stroke rehabilitation (rehab) is a critical part of a successful recovery. Early rehab, begun as soon as possible after the stroke, helps to reduce dependence on others. Most recovery occurs during the first 3 months after a stroke but may continue slowly over the next few years. For more information, see the topic Stroke Rehabilitation.
One of the foremost rehabilitation devices for post stroke recovery is the Tutor system.
The Tutor system, consisting of the HandTutor, ArmTutor, LegTutor and 3DTutor, has been developed to allow for functional rehabilitation of the whole body including the upper and lower extremity. The system consists of ergonomic wearable devices and dedicated rehabilitation software that provide patient instructions and feedback to encourage intensive massed controlled exercise practice. The Tutor system allows for controlled exercise of multijoints within the normal movement pattern which prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks. Additional features of the Tutor system include quantitative evaluation, objective follow up and tele-rehabilitation.
The new medical devices are available for children as well as adults and through the use of telerehabilitation and are FDA and CE certified.
Tutors Accelerate Therapy Treatment Following Stroke

The following are important facts from the National Stroke Association:
Thrombolytics
Thrombolytic (fibrinolytic) drugs help reestablish blood flow to the brain by dissolving the clots, which are blocking the flow. In June, 1996, the “clot-buster” Activase® (Alteplase recombinant) became the first acute ischemic stroke treatment to be approved by the Federal Food and Drug Administration (FDA). Activase is also known as tissue plasminogen activator (tPA). To be effective, thrombolytic therapy should be given as quickly as possible.
tPA
tPA is an enzyme found naturally in the body that converts, or activates, plasminogen into another enzyme to dissolve a blood clot. It may also be used in an IV by doctors to speed up the dissolving of a clot. tPA should be given within three hours of symptom onset. It is important for people to understandstroke warning signs and get to a hospital FAST in case they are eligible to receive tPA. Time is an important factor associated with determining whether a patient can receive it or not.
The results of a five-year trial, conducted by the National Institute of Neurological Disorders and Stroke (NINDS) found that carefully selected stroke patients who received Activase within three hours of the beginning of stroke symptoms were at least 33 percent more likely than patients given a placebo to recover from their stroke with little or no disability after three months. The most common complication associated with Activase is brain hemorrhage. However, studies have shown that tPA does not increase the death rate of stroke patients when compared with placebo.
MERCI Retrieval System
In 2004 the FDA cleared Concentric Medical’s innovative Merci® Retriever for patients who are ineligible for IV-tPA or fail to respond to IV-tPA. The system can be used for patients who are beyond the 3-hour time window for IV-tPA and it does not have a time limit for its intended use. This device offers physicians and patients long-awaited options for stroke intervention and creates a departure from the historic method of caring for stroke patients. The Merci Retriever has repeatedly been proven to restore blood flow in the larger vessels of the brain by removing blood clots. Over 8,000 patients world-wide have undergone this procedure and it has been performed at over 300 US hospitals. The system is a tiny cork-screw shaped device that works by wrapping around the clot and trapping it. The clot is then retrieved and removed from the body.
The newly developed Tutor system (HandTutor, ArmTutor, LegTutor and 3DTutor) is foremost amongst the primary rehabilitation devices for post stroke recovery.
These innovative devices are used for TBI, SCI, Parkinson’s, CP, limb and joint surgery, Complex Regional Pain Syndrome, shoulder pain, locked joints and other disabilities. The Tutors implement an impairment based program with augmented feedback. They encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient’s performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient’s ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation.
Wednesday 26 October 2011
Crash Victim Adams Can Benefit From the LegTutor

Danny Hall writes in the Wilts and Gloucesteshire on Oct.26, 2011 about the SWINDON speedway legend Leigh Adams who checked in to the Project Walk Spinal Cord Injury Recovery Clinic in California on January 1 as he bids to get his life back on track in the wake of the off road motor cycle crash on June 7 that has left him in a wheelchair.
In his first major radio interview with BBC Wiltshire’s award-winning Graham Mack, Adams said: “It is an eight-week spin in California. We’ve heard great things about the place and we are going to throw everything at it.”
Adams, 40, has been inspired by the recovery of former Danish speedway world champion Eric Gundersen, who had to learn to walk again after being involved in a race crash that left him in a coma, and also by an unnamed Australian snowboarder.
“Eric is unbelievable – an inspiration,” said Adams. “He was quadriplegic so quite a lot worse than me.
“I have also been in touch with a snowboarder over here (Australia) who recovered to walk again having gone to the (Project Walk) clinic.”
When asked whether he would ever walk again, Adams said: “If we had a crystal ball, that would be fantastic.
“It’s going to be a bit of luck; it’s mental strength and putting everything into it.
“It will be a two-year period, that’s when the bulk of the repair comes from. It’s expensive, but I want to tick every box that I can.”
Adams has already made plenty of progress.
He said “I don’t remember a thing abut the crash. It was only a couple of days later when I came to that there was no feeling in my legs.
“We’re not kicking any goals, but we are going forward “We’ve got pretty good movement in the left leg, the right leg is very slowly coming along.
“The left one has always been ahead. When I came out of hospital I had pins and needles in my left leg and now there is pretty much full movement in it. Now we have to try and build muscle.”
Adams was quick to praise the role of his family in his rehabilitation, particularly his wife Kylie.
He said: “Kylie was the rock behind me when I was racing and she still is now.”
The speedway community has got behind Adams in an effort to raise money for his very expensive treatment in the States.
There is a Benefit Meeting at Gillman Speedway in Adelaide on November 26, all proceeds to go to the Leigh Adams Rehabilitation Fund.
“The support from the speedway world has blown me away,” he said. “I had planned to come back to England in 2012 and take in the Olympics but that is on the back burner for a while.
“But we will be back, even if it takes a bit of time.”
The LegTutor will be of great assistance to Leigh Adams in his recovery from the crash as it improves functional outcomes in physical rehabilitation.
The LegTutor™ system has been developed to allow for functional rehabilitation of the lower extremity. The system consists of an ergonomic wearable leg brace and dedicated rehabilitation software. The LegTutor™ system allows for a range of biomechanical evaluation including speed, passive and active range of motion and motion analysis of the lower extremity. Quantitative biomechanical data allow for objective evaluation and rehabilitation treatment follow up. The LegTutor™ rehabilitation concept is based on performing controlled exercise rehabilitation practice at a patient customized level with real time accurate feedback on the patient’s performance. The exercises are designed in the form of challenging games that are suitable for a wide variety of neurological and orthopedic injury and disease.
The games challenge the patient to perform the exercise task to their best ability and to continue exercise practice.
The LegTutor™ allows for isolated and a combination of knee and three directional hip treatment. The system provides detailed exercise performance instructions and precise feedback on the patients exercise performance. Controlled exercise of multi joints within the normal movement pattern prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks.
The LegTutor™ system is used by many leading rehabilitation centers worldwide and has full FDA and CE certification The Tutors (HandTutor, ArmTutor, LegTutor and 3DTutor are available for children as well as adults and can be used at home vis telerehabilitation. .
.
The Tutor System Maintains Current Strength in Osteoarthritis Patients

Susan Hill et al in a study for Disability and Rehabilitation, December 2011 discuss a study whose purpose is to describe. Osteoarthritis (OA) as the commonest reason for a musculoskeletal consultation in primary care in older adults. There is evidence that appropriate advice and management is sub-optimal. The aim of this study was to explore perceptions and experiences of the treatment and management of hand OA in older adults.
The methods used in the study were four focus groups who were conducted with primary (n === 15) and secondary (n === 14) care participants aged 50-84 years (mean age 64.9 years; 3 males, 14 females) with a clinical diagnosis of hand OA. Data were tape-recorded, transcribed and analysed using thematic analysis and constant comparison method.
The results showed that participants described a lack of help and information with regards to management of their hand OA and also a perceived lack of understanding of the impact of hand OA on the individual. Some received contradictory advice about its management. Beliefs about treatment efficacy were balanced against perceived and actual side-effects and tolerance, and such perceptions appeared to influence the use of alternative therapies.
The conclusions reached were that the study identified a perceived unmet need in people with hand OA presenting in primary and secondary care. This may be due to the clinical uncertainty of treatment, lack of high-quality randomised controlled trials evaluating therapeutic options, and the limited written information available incorporating the patient experience. The study emphasised the need to understand patient illness and treatment beliefs. A better understanding of illness and treatment beliefs will facilitate the use of evidence-based approaches in the management of hand OA.
The Tutor devices provide for interactive rehabilitation exercises and can alleviate some of the shoulder and other joint pain.
The Tutor system, consisting of the HandTutor, ArmTutor, LegTutor and 3DTutor, has been developed to allow for functional rehabilitation of the whole body including the upper and lower extremity. The system consists of ergonomic wearable devices and dedicated rehabilitation software that provide patient instructions and feedback to encourage intensive massed controlled exercise practice. The Tutor system allows for controlled exercise of multijoints within the normal movement pattern which prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks. Additional features of the Tutor system include quantitative evaluation, objective follow up and tele-rehabilitation.
The new medical devices are available for children as well as adults and through the use of telerehabilitation and are FDA and CE certified.
Tutor System Complements Breathing Therapy for SCI Patients

Maureen McFadden reporting in WNDU.COM, October, 2011 files this story.
Every year, more than 10,000 Americans suffer a spinal cord injury.
For some, it means total paralysis, for others, it’s all about finding treatments that can help improve their strength and function. Now, an experimental rehab therapy has patients breathing their way to recovery.
27-year-old Drew Durrence is all about overcoming challenges. Eight years ago, he injured his spinal cord in a dirt bike accident.
Drew Durrence, injured spinal cord, describes when he first realized something was wrong, “When I tried to get up, I lost feeling and movement from about chest down.”
Therapy, and Drew’s determination, have brought some of that back. Now, he’s part of a unique trial.
Physical therapist and biomedical engineer Doctor Randy Trumbower is studying how oxygen deprivation can trigger molecular changes that excite, or wake up, the nervous system.
Randy Trumbower, PHD Assistant Professor, Rehabilitation Medicine Emory University School of Medicine, describes the treatment, “And so what we’re hoping is that by intermittently stimulating the spinal cord with this type of breathing intervention, that we’re actually turning up the volume on spared connections.”
Patients alternately breathe air with low, nine percent oxygen and normal, 21 percent oxygen.
Trumbower, explains some of the results of the treatment, “We found that individuals that experienced intermittent hypoxia for one day, for 45 minutes of exposure actually increased, on average, 80 percent changes in strength.”
In early trials, this oxygen deprivation therapy also helped patients use muscles they couldn’t use before.
Durrence, describes how the treatment has helped him in his everyday life, “If you can get just a little bit more strength where it makes it easier for you to stand up, or easier for you to do something, that’s just another step.”
Whatever it takes, Drew says he’ll keep challenging himself to do more, taking control of his injury, instead of letting it control him.
Patients who had the therapy for seven consecutive days had improvements in strength that lasted for a month or more.
This trial has been going on since last year and is still recruiting patients in the Atlanta area for further studies.
A spinal cord injury often causes permanent disability or loss of movement and sensation below the site of the injury. The ability to control limbs depends on two factors: the neurological level of the injury, which is the lowest functioning segment of the spinal cord, and the completeness of the injury. An injury is considered complete if all sensory and motor function is lost below the neurological level. The injury is incomplete if there is still some sensory and motor function below the injury site. Symptoms of spinal cord injuries include loss of movement; loss of the ability to feel heat or cold; loss of touch; difficulty breathing; coughing; and loss of bowel or bladder control. (SOURCE: Mayo Clinic)
A traumatic blow to the spine that fractures, dislocates, crushes or compresses one or more of the vertebrae can cause a spinal cord injury. The nerve fibers that pass through the injured area are affected, and therefore, may impair part or all of the corresponding muscles and nerves below the site of the injury. Other causes of spinal cord injury include a gunshot or knife wound that penetrates and cuts the spinal cord. Arthritis, cancer, inflammation, infections, or disc degeneration of the spine can also cause spinal cord injury. (SOURCE: Mayo Clinic)
The new therapy for spinal cord injuries uses oxygen deprivation in order to trigger molecular changes that excite or awaken the nervous system. The therapy uses acute intermittent hypoxia, which has its roots in sleep apnea studies. People with sleep apnea undergo short periods of oxygen deprivation, which stimulates spinal plasticity — the ability of the brain and nervous system to respond to experience or injury. Intermittent hypoxia was tested on subjects who had been paralyzed, by placing a breathing mask on them that was connected to an air generator that stimulates the air at the peak of Mount McKinley then returns the air to normal. Nerve cells associated with voluntary leg strength were stimulated through a 30-minute mild oxygen deprivation session, resulting in improved ankle strength that lasted four hours.
The Tutors (HandTutor, ArmTutor, LegTutor and 3DTutor) present an excellent supplement to the oxygen deprivation system for SCI patients. The Tutors have shown improvement in range of motion for patients suffering from incomplete paralysis. They are challenging and present a way to give more strength to the recovering patient.
These innovative devices implement an impairment based program with augmented feedback and encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient’s performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient’s ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation.
Tuesday 25 October 2011
Tutor System Increases Confidence and Sense of Achievement for SCI Patients

As reported by Chris Thomas in SCIENCE NETWORK in Western Australia on October 25, 2011
An innovative rehabilitation program has been introduced to Edith Cowan University’s Joondalup campus, after the establishment of a partnership with Spinal Cord Injuries Australia.
“The program aims to give the nervous system a chance to reactivate below the level of injury.”said therapist Kierre Ireland.
Funded by a $320,000 Lotterywest grant, the ‘Walk On Program’ is based at ECU’s Health and Wellness Institute with staff and students trained to develop specific rehabilitation exercises while using state-of-the-art equipment
About 50 people receive a spinal cord injury every year in WA, in addition to the thousands already living with a spinal cord injury.
Twelve people have been chosen to take part in an individually designed exercise program to help maximise their functional recovery.
National Walk On therapist Kierre Ireland says it is a chance for them to get out of their wheelchairs for a two-hour session and complete whole body, intensive and dynamic exercises—no matter what level of function they may have.
“We work all parts of the body, not just the areas unaffected by the injury,” she says.
“This aims to give the nervous system a chance to reactivate below the level of injury.
“All clients complete exercises in different positions, from lying on their side or tummy, to kneeling, standing, crawling and even walking.
“Many clients report the variety of exercises and positions gives them an increased confidence and awareness of their body once again, as well as a sense of achievement and overall positive outlook on their lives.”
Three exercise physiologists completed six weeks of training in activity-based spinal cord injury therapy at the University of Sydney and the Project Walk SCI recovery centre in Carlsbad, California, before the program was launched.
Ms Ireland says the training exposes them to a broad variety of people with different levels and severity of injuries.
“A spinal cord injury is such an individualised injury, meaning there are rarely two people who present with the same level of function and ability,” she says.
“There is no other training in the neurological field that offers such an extended experience and exposure working exclusively with people with spinal cord injuries.”
Physical benefits include an improvement in patients’ ability to transfer from wheelchairs to beds or in and out of cars, being able to wash or feed themselves more independently and an overall improvement in balance and strength that makes it easier for them to pick things up.
“Many of our clients also report gaining a huge psychological improvement with a more positive approach to their lives, increase in self-confidence and a sense of worth,” Ms Ireland says.
The newly developed state of the art Tutor devices have through their powerful evaluation software increased the confidence and sense of achievement of patients suffering from SCI, Brain injury, Parkinson’s disease, MS, stroke, limb surgery and other debilitating issues. The Tutor system (HandTutor, ArmTutor, LegTutor and 3DTutor) are designed to give the patient a functional recovery. The 3DTutor, for example, is a wireless motion feedback device that can be positioned on discrete joints of the head, trunk or upper and lower extremities. This allows for evaluation and treatment of the joint of choice. The 3D unit can be used independently or in conjunction with the other Tutor devices to exercise interjoint movements. The Tutor system can bring a positive approach to the life of the patient.
The HandTutor and its “sisters” is currently being used successfully in leading U.S. and foreign hospitals and clinics. It is designed for adults and children alike and is fully certified by the FDA and CE.
U.S.Rep.Giffords Can Supplement her Therapy With the Tutor System

ASHEVILLE — Since the late 1800s, Asheville has been known nationwide as a rehabilitation haven. So, in a way it should come as no big surprise that U.S. Rep. Gabrielle Giffords is spending the next two weeks here for intensive work with an Asheville therapist.
“It’s something that’s been planned for quite some time — it’s not a last-minute thing,” said Mark Kimble, spokesman for Giffords, D-Ariz. “It’s also just an attempt to have a period of very focused and concentrated therapy with this therapist. It’s part of her continuing recovery in a number of different areas.”
Giffords was shot in the head Jan. 8 at an event in Arizona, surviving an injury to her brain that leaves 88 percent of victims dead. She can understand written and spoken language, but still has some trouble speaking, especially when she’s tired or under stress, Kimble said.
He declined to state who the Asheville therapist is but said the person has been working regularly with Giffords during her nine-month rehabilitation in Houston.
Asheville’s reputation as a rehabilitation center dates to the 19th century when hundreds of tuberculosis patients came here for the rejuvenating mountain air. In the 20th and 21st centuries, much of that reputation has revolved around CarePartners Rehabilitation Hospital, an 80-bed regional center with rehabilitation programs for a numerous illnesses, injuries and conditions.
Opened in 1938, the facility formerly was called Thoms Rehabilitation Hospital and has drawn severely injured patients to the mountains for decades.
CarePartners does not have a patient by the name Gabrielle Giffords, said Tom Adkins, vice president of business development. Merrell Gregory, a spokeswoman at Mission Health, which has an outpatient rehabilitation operation, also said the hospital has no patients by that name.
Like all members of Congress, Giffords is under the security protection of the U.S. Capitol Police. She has no public appearances scheduled here, Kimble said. The therapy will be intensive, though.
If the Asheville rehabilitation center that the congresswoman is receiving physical therapy in includes the Tutor system her progress will be enhanced by it.
The Tutor system, consisting of the HandTutor, ArmTutor, LegTutor and 3DTutor, has been developed to allow for functional rehabilitation of the whole body including the upper and lower extremity. The system consists of ergonomic wearable devices and dedicated rehabilitation software that provide patient instructions and feedback to encourage intensive massed controlled exercise practice. The Tutor system allows for controlled exercise of multijoints within the normal movement pattern which prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks. Additional features of the Tutor system include quantitative evaluation, objective follow up and tele-rehabilitation.
The new medical devices are available for children as well as adults and through the use of telerehabilitation and are FDA and CE certified.
Monday 24 October 2011
Tutor System Speeds Brain Injury Recovery of Upper As Well As Lower Joints

As announced on PR WEB in October 2011, Encore Path, makers of the Tailwind device for arm rehabilitation for stroke and brain injury survivors announced its invitation to join Astia, the premier global network serving women-led high growth start-ups since 1999.
Encore Path develops rehabilitation devices for stroke and brain injury survivors. Its first product, the Tailwind, was released in 2009. It is clinically proven to help people with moderate to severe paralysis improve their arm function and range of motion. The Tailwind is available in rehabilitation hospitals and therapy centers worldwide, and is also sold to patients who want to use it at home.
The Tailwind was developed by University of Maryland doctors specializing in physical therapy rehabilitation after a decade of scientific research. Clinical studies have shown that the device helps improve arm mobility, function, and range of motion in patients with even severe paralysis.
The Tutor system (HandTutor, ArmTutor, LegTutor, 3DTutor) uses augmented movement feedback, and allows for customizable and motivating exercise practice for all joints (and not just elbow and arm) and allows the training of two associated joints in a functional movment e.g elbow and shoulder. The Tutor system uses augmented feedback to prevent the patient using a compensatory movement pattern to achieve the task.
The Tutor system can also be used for open and closed chain movement practice in the sitting, standing and lying position.
The system consists of motivating and challenging games that allow the patient to practice isolated and/or interjoint coordination exercises so as not to become bored with the therapy. Controlled exercise practice helps to prevent the development of compensatory movement patterns. The dedicated software allows the therapist to fully customize the exercises to the patient’s movement ability. In addition the therapist can objectively and quantitatively evaluate and report on the treatment progress. The rehabilitation system optimizes the patient’s motor, sensory and cognitive performance and allows the patient to better perform everyday functional tasks to improve their quality of life. The Tutor system is FDA and CE certified and can be used at home via telerehabilitation.
LegTutor an Important Boost for People With Stiff-Knee Gait Following Stroke

Dr. James S. Sulzer from the Rehabilitation Institute of Chicago Chicago, Ill; the Departments of Mechanical and Biomedical Engineering, Northwestern University, Evanston, Ill; and the Department of Bioengineering, University of Illinois–Chicago, Chicago, Ill.writing for the American Heart and Stroke Associations made the following study:
Background and Purpose— Stiff-knee gait is defined as reduced knee flexion during the swing phase. It is accompanied by frontal plane compensatory movements (eg, circumduction and hip hiking) typically thought to result from reduced toe clearance. As such, we examined if knee flexion assistance before foot-off would reduce exaggerated frontal plane movements in people with stiff-knee gait after stroke.
Methods— We used a robotic knee orthosis to assist knee flexion torque during the preswing phase in 9 chronic stroke subjects with stiff-knee gait on a treadmill and compared peak knee flexion, hip abduction, and pelvic obliquity angles with 5 nondisabled control subjects.
Results— Maximum knee flexion angle significantly increased in both groups, but instead of reducing gait compensations, hip abduction significantly increased during assistance in stroke subjects by 2.5°, whereas no change was observed in nondisabled control subjects. No change in pelvic obliquity was observed in either group.
Conclusions— Hip abduction increased when stroke subjects received assistive knee flexion torque at foot-off. These findings are in direct contrast to the traditional belief that pelvic obliquity combined with hip abduction is a compensatory mechanism to facilitate foot clearance during swing. Because no evidence suggested a voluntary mechanism for this behavior, we argue that these results were most likely a reflection of an altered motor template occurring after stroke.
The LegTutor has proven to be an important complement in improving functional outcomes in physical rehabilitation for post stroke patients.
The LegTutor provides a safe and comfortable leg brace with position and speed sensors that precisely record three dimensional hip and knee extension, flexion and hip abduction. Rehabilitation games allow the patient to exercise Range of Motion (ROM), speed and accuracy of movement. The LegTutor facilitates evaluation and treatment of the lower extremity including isolated and combined hip and knee movements.
The LegTutor together with its sister devices (HandTutor, ArmTutor and 3DTutor) aim to optimize motor, sensory and cognitive performance to allow the patient to better perform everyday functional tasks through interactive rehabilitation exercises in order to improve quality of life. The Tutors are being successfully used in leading U.S. and foreign hospitals and clinics and are suitable for home use through telerehabilitation. They are available for children as well as adults.
Post Knee Replacement Surgery Involves Use of the LegTutor

Vikki Petersen writing in Health Now October 2011 states that baby boomers are getting older. With increased age comes increased wear and tear on the joints of the body, but the desire to remain active has resulted in more and more surgeons and patients opting for knee replacements than ever before. Unfortunately most patients are told only about how the surgery helps in decreasing pain levels and assists them in getting back to their active lifestyle. Very few are actually told the realities of how important rehab is or how difficult it can be to truly regain full range of motion or strength in the replaced knee. As a physical therapist I too often see patients coming in for a post surgery appointment with absolutely no idea of what it will take to restore their knee back to the flexibility and strength they desire.
If the post knee surgery rehabilitation involves the LegTutor™ the chances of returning full range of motion are increased manyfold.
The LegTutor™ system has been developed to allow for functional rehabilitation of the lower extremity. The system consists of an ergonomic wearable leg brace and dedicated rehabilitation software. The LegTutor™ system allows for a range of biomechanical evaluation including speed, passive and active range of motion and motion analysis of the lower extremity. Quantitative biomechanical data allow for objective evaluation and rehabilitation treatment follow up. The LegTutor™ rehabilitation concept is based on performing controlled exercise rehabilitation practice at a patient customized level with real time accurate feedback on the patient’s performance. The exercises are designed in the form of challenging games that are suitable for a wide variety of neurological and orthopedic injury and disease.
The games challenge the patient to perform the exercise task to their best ability and to continue exercise practice.
The LegTutor™ allows for isolated and a combination of knee and three directional hip treatment. The system provides detailed exercise performance instructions and precise feedback on the patients exercise performance. Controlled exercise of multi joints within the normal movement pattern prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks.
The LegTutor™ system is used by many leading rehabilitation centers worldwide and has full FDA and CE certification.
Neuroplasticity and its Applications for Rehabilitation With the Tutor System
Posted January 13, 2011
Image via Wikipedia
Neuroplasticity and its applications for rehabilitation using the Tutor system:
In the January edition of theAmerican Journal of Therapeutics Symposium: Stroke Management, Dr. Young and Dr. Tolentino of Rush University report on neuroplasticityand its applications for rehabilitationhttp://bit.ly/gN0oUW . The report describes the various studies on neuro plasticity and the variety of interventions now available.
The HandTutor system with its sister devices (ArmTutor, LegTutor and 3DTutor) uses the proven concept of active intensive exercise practice. However the power of the dedicated rehabilitation software is the fact the exercise task provides the patient with real time instructions on how to move their hand, arm, fingers and other joints of the body. The tasks can be customized so that the difficulty level will exercise the patients exact movement dysfunction. In addition augmented feedback is provided on the result of the patient’s movement and on the patients movement performance this motivates and stimulate patients to continue task practice.
www.HandTutor.com
Sunday 23 October 2011
LegTutor Enhances Range of Motion for Knee Replacement Patients

Pazit Levinger etal conducted a study published in Springer Link in October 2011.
The purpose of the study was to determine why knee pain and disability persists following knee replacement surgery which may place patients at increased risk of falls. This study investigated the falls risk and the occurrence of falls of people with knee osteoarthritis (OA) before and at 12 months following knee replacement surgery.
The method used in the study was:
Thirty-five patients with knee OA were tested prior to undergoing knee replacement surgery and at 12 months following surgery using the short form Physiological Profile Assessment, which incorporates tests of vision, lower limb proprioception, knee extension strength, reaction time and postural sway. Physical activity, number of falls, fear of falling, pain, disability and health-related quality of life were also assessed.
The results showed that there were no significant differences found between the number of falls pre- and post-surgery (n.s.), with 48.5 and 40% reporting at least one fall in the 12 months before and following the surgery, respectively. Improvements in knee strength, reaction time and fear of falling were evident following surgery, with no improvement in lower limb proprioception. Self-reported pain, function and stiffness were significantly improved, but health-related quality of life deteriorated following the surgery.
The conclusion reached was that the number of falls experienced following knee replacement surgery remained relatively high, which may be attributed to the persistence of impaired lower limb proprioception. Although knee replacement surgery improves function and alleviates pain, people who undergo this procedure may need to engage in rehabilitation following the surgery to reduce the risk of falling.
The LegTutor has shown remarkable success in post knee replacement surgery. The LegTutor™ system has been developed to allow for functional rehabilitation of the lower extremity. The system consists of an ergonomic wearable leg brace and dedicated rehabilitation software. The LegTutor™ allows for a range of biomechanical evaluation including speed, passive and active range of motion and motion analysis of the lower extremity. Quantitative biomechanical data allow for objective evaluation and rehabilitation treatment follow up. The LegTutor™ rehabilitation concept, which includes the HandTutor, ArmTutor and 3DTutor, is based on performing controlled exercise rehabilitation practice at a patient customized level with real time accurate feedback on the patient’s performance. The exercises are designed in the form of challenging games that are suitable for a wide variety of neurological and orthopedic injury and disease.The games challenge the patient to perform the exercise task to their best ability and to continue exercise practice.
The LegTutor™ allows for isolated and a combination of knee and three directional hip treatment. The system provides detailed exercise performance instructions and precise feedback on the patients exercise performance. Controlled exercise of multi joints within the normal movement pattern prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks.
The LegTutor™ system is used by many leading rehabilitation centers worldwide and has full FDA and CE certification and is available for adults and children.
Tutor System Available by Telerehabilitation
As posted on 10/21/2011 by the University of California System: University of California, Irvine:
To regain movement and mobility after a stroke, stroke patients undergo intensive rehabilitative therapy with rehabilitation nurses and physical therapists. These rehabilitation sessions occur on an outpatient basis and typically average three days a week for several hours a day. Such sessions are expensive since it involves one-on-one therapy sessions between the patient and the therapist. It also may be inconvenient for a stroke patient to travel to the rehabilitation sessions, particularly given post-stroke disabilities or regional disparities in health resources. Furthermore, studies have shown that a larger dose of rehabilitation therapy can be beneficial for the stroke patient. A physician at the University of California, Irvine has developed a new telerehabilitation system including new software that may be used or supplemented in stroke patients’ rehabilitation therapy programs. This telerehabilitation system may be used at home and would cost significantly less than physical therapy and eliminate the patient’s commute to a therapy session.
Stroke patients as well as those who have had a TBI or Spinal cord injury can, when they are sufficiently recovered, avail themselves of the Tutor system through the use of telerehabilitation.
The HandTutor, ArmTutor, LegTutor and 3DTutor have been developed to allow for functional rehabilitation of the whole body including the upper and lower extremity. The system consists of ergonomic wearable devices and dedicated rehabilitation software that provide patient instructions and feedback to encourage intensive massed controlled exercise practice. The Tutor system allows for controlled exercise of multijoints within the normal movement pattern which prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks. Additional features of the Tutor system include quantitative evaluation and objective follow up. The Tutors are FDA and CE certified.The new medical devices are available for children as well as adults.
To regain movement and mobility after a stroke, stroke patients undergo intensive rehabilitative therapy with rehabilitation nurses and physical therapists. These rehabilitation sessions occur on an outpatient basis and typically average three days a week for several hours a day. Such sessions are expensive since it involves one-on-one therapy sessions between the patient and the therapist. It also may be inconvenient for a stroke patient to travel to the rehabilitation sessions, particularly given post-stroke disabilities or regional disparities in health resources. Furthermore, studies have shown that a larger dose of rehabilitation therapy can be beneficial for the stroke patient. A physician at the University of California, Irvine has developed a new telerehabilitation system including new software that may be used or supplemented in stroke patients’ rehabilitation therapy programs. This telerehabilitation system may be used at home and would cost significantly less than physical therapy and eliminate the patient’s commute to a therapy session.
Stroke patients as well as those who have had a TBI or Spinal cord injury can, when they are sufficiently recovered, avail themselves of the Tutor system through the use of telerehabilitation.
The HandTutor, ArmTutor, LegTutor and 3DTutor have been developed to allow for functional rehabilitation of the whole body including the upper and lower extremity. The system consists of ergonomic wearable devices and dedicated rehabilitation software that provide patient instructions and feedback to encourage intensive massed controlled exercise practice. The Tutor system allows for controlled exercise of multijoints within the normal movement pattern which prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks. Additional features of the Tutor system include quantitative evaluation and objective follow up. The Tutors are FDA and CE certified.The new medical devices are available for children as well as adults.
Saturday 22 October 2011
Tutor System Can Augment Proposed Medication
The following was published in The Sacramento Bee on Friday, Oct. 21, 2011:
Avanir Pharmaceuticals, Inc. today announced that pseudobulbar affect (PBA) prevalence data from stroke survivors will be highlighted at the 88th Annual Meeting of the American Congress of Rehabilitation Medicine/American Society for Neurorehabilitation Medicine in Atlanta, GA.
Following are details about the data presentation at ACRM/ASNR Progress in Rehabilitation Research:
Title: Pseudobulbar Affect in Stroke: A National Stroke Association SurveyProgram Number: 0025 Presentation Date/Time: Thursday, October 13, 2011 5:00-7:00 p.m. EST & Friday October 14, 2011 4:30-6:45 p.m. EST
What is PBA?
Patients suffering from existing neurological disease or brain injury may also suffer the added burden of pseudobulbar affect, or PBA. PBA occurs secondary to a variety of otherwise unrelated neurological conditions, and is characterized by involuntary, sudden, and frequent episodes of crying and/or laughing. PBA episodes typically occur out of proportion or incongruent to the patient’s underlying emotional state. PBA outbursts result from a “short circuit” in the brain caused by another neurologic condition-such as multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS), stroke, or traumatic brain injury. PBA can have a debilitating impact on the lives of patients, caregivers and loved ones.
The dose and timing of Avanir’s proposed medication to counteract PBA can augment functional gain of physiotherapy. The Tutor system has been effective as a physical therapist’s tool for patients recovering from brain and spinal cord injury, MS, ALS and other debilitating diseases.
These innovative devices, known as the HandTutor, ArmTutor, LegTutor and 3DTutor, implement an impairment based program with augmented feedback and encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient’s performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient’s ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation.
Avanir Pharmaceuticals, Inc. today announced that pseudobulbar affect (PBA) prevalence data from stroke survivors will be highlighted at the 88th Annual Meeting of the American Congress of Rehabilitation Medicine/American Society for Neurorehabilitation Medicine in Atlanta, GA.
Following are details about the data presentation at ACRM/ASNR Progress in Rehabilitation Research:
Title: Pseudobulbar Affect in Stroke: A National Stroke Association SurveyProgram Number: 0025 Presentation Date/Time: Thursday, October 13, 2011 5:00-7:00 p.m. EST & Friday October 14, 2011 4:30-6:45 p.m. EST
What is PBA?
Patients suffering from existing neurological disease or brain injury may also suffer the added burden of pseudobulbar affect, or PBA. PBA occurs secondary to a variety of otherwise unrelated neurological conditions, and is characterized by involuntary, sudden, and frequent episodes of crying and/or laughing. PBA episodes typically occur out of proportion or incongruent to the patient’s underlying emotional state. PBA outbursts result from a “short circuit” in the brain caused by another neurologic condition-such as multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS), stroke, or traumatic brain injury. PBA can have a debilitating impact on the lives of patients, caregivers and loved ones.
The dose and timing of Avanir’s proposed medication to counteract PBA can augment functional gain of physiotherapy. The Tutor system has been effective as a physical therapist’s tool for patients recovering from brain and spinal cord injury, MS, ALS and other debilitating diseases.
These innovative devices, known as the HandTutor, ArmTutor, LegTutor and 3DTutor, implement an impairment based program with augmented feedback and encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient’s performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient’s ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation.
Friday 21 October 2011
Occupational Therapists Can Boost their Success with the Tutor System
Rebekah Polley writing in the Central Queensland News on 21st October 2011 about Roslyn Core who is passionate about her work as an occupational therapist.
For occupational therapist Roslyn Core, her job is about the individual moments.
It is those individual moments that make Roslyn passionate about her job as next week marks OT Week where occupational therapists across Australia are celebrated for the work they do.
Roslyn works for Education Queensland and her role involves helping children participate in everyday activities at school and in the community, and achieve developmental milestones such as fine motor skills and hand-eye co-ordination.
“It’s hands on, challenging and varying,” Roslyn said of her job.
“When you see kids make those milestones, it’s very rewarding.
“So many of the children surprise you every day with what they achieve.”
Roslyn has been an occupational therapist for nearly four years and became interested in the profession after her cousin studied the course at university and enjoyed it.
“I fell into it more than chose it,” she said with a laugh.
“I enjoyed the first year and kept doing it.
“There is a huge variety of things you can do with one degree.”
Roslyn studied at James Cook University in Townsville and after working in Roma, got transferred back home to Emerald.
“Emerald is home as I grew up here,” she said.
“I love the community and the people. I prefer to live in country towns.”
Roslyn said she meets some “amazing people” through her job and is taking her skills overseas for a couple of years.
“I want to do something similar overseas and come back and continue my work,” she said.
OT Week is also about spreading awareness about the work occupational therapists do and Roslyn encouraged anyone interested in the profession to find out more.
“If you have a passion for helping other people then definitely do it,” she said.
“It’s an amazing job.”
Occupational therapists using the Tutor system for rehabilitative work find their work much easier to perform.
The Tutor system (HandTutor, ArmTutor, LegTutor, 3DTutor) has shown much success in rehabilitation of joint movement. The newly developed Tutors consist of ergonomic wearable devices together with powerful dedicated rehabilitation software. The system is indicated for patients to be used by occupational therapists and physiotherapists in rehabilitation centers, private clinics and the home where it can be supported by telerehabilitation. It is designed for those who have head, trunk, upper and lower extremity movement dysfunction.
The system consists of motivating and challenging games that allow the patient to practice isolated and/or interjoint coordination exercises. Controlled exercise practice will help to prevent the development of compensatory movement patterns. The dedicated software allows the therapist to fully customize the exercises to the patient’s movement ability. In addition the occupational therapist can objectively and quantitatively evaluate and report on the treatment progress. The rehabilitation system optimizes the patient’s motor, sensory and cognitive performance and allows the patient to better perform everyday functional tasks to improve their quality of life. The Tutor system is FDA and CE certified.
For occupational therapist Roslyn Core, her job is about the individual moments.
It is those individual moments that make Roslyn passionate about her job as next week marks OT Week where occupational therapists across Australia are celebrated for the work they do.
Roslyn works for Education Queensland and her role involves helping children participate in everyday activities at school and in the community, and achieve developmental milestones such as fine motor skills and hand-eye co-ordination.
“It’s hands on, challenging and varying,” Roslyn said of her job.
“When you see kids make those milestones, it’s very rewarding.
“So many of the children surprise you every day with what they achieve.”
Roslyn has been an occupational therapist for nearly four years and became interested in the profession after her cousin studied the course at university and enjoyed it.
“I fell into it more than chose it,” she said with a laugh.
“I enjoyed the first year and kept doing it.
“There is a huge variety of things you can do with one degree.”
Roslyn studied at James Cook University in Townsville and after working in Roma, got transferred back home to Emerald.
“Emerald is home as I grew up here,” she said.
“I love the community and the people. I prefer to live in country towns.”
Roslyn said she meets some “amazing people” through her job and is taking her skills overseas for a couple of years.
“I want to do something similar overseas and come back and continue my work,” she said.
OT Week is also about spreading awareness about the work occupational therapists do and Roslyn encouraged anyone interested in the profession to find out more.
“If you have a passion for helping other people then definitely do it,” she said.
“It’s an amazing job.”
Occupational therapists using the Tutor system for rehabilitative work find their work much easier to perform.
The Tutor system (HandTutor, ArmTutor, LegTutor, 3DTutor) has shown much success in rehabilitation of joint movement. The newly developed Tutors consist of ergonomic wearable devices together with powerful dedicated rehabilitation software. The system is indicated for patients to be used by occupational therapists and physiotherapists in rehabilitation centers, private clinics and the home where it can be supported by telerehabilitation. It is designed for those who have head, trunk, upper and lower extremity movement dysfunction.
The system consists of motivating and challenging games that allow the patient to practice isolated and/or interjoint coordination exercises. Controlled exercise practice will help to prevent the development of compensatory movement patterns. The dedicated software allows the therapist to fully customize the exercises to the patient’s movement ability. In addition the occupational therapist can objectively and quantitatively evaluate and report on the treatment progress. The rehabilitation system optimizes the patient’s motor, sensory and cognitive performance and allows the patient to better perform everyday functional tasks to improve their quality of life. The Tutor system is FDA and CE certified.
Wednesday 19 October 2011
Rehabilitation Facilities Using Tutor System Amongst the Best

BOSTON, Oct. 18, 2011 /PRNewswire via COMTEX/ — A life-altering event, followed by a miraculous recovery. This is the story of Gabrielle Giffords, the U.S. House of Representatives member who recovered from a near-fatal gunshot head wound. Most Americans will never face a similar fate, however, other medical conditions – including stroke, brain and spinal cord injury, neurological disorders (like Parkinson’s disease and multiple sclerosis), complex orthopedic issues, and amputation – will require intensive rehabilitative therapy. For those affected, the question becomes, Will I receive the same quality of care as Gabrielle Giffords?
When preparing to leave a hospital’s Intensive Care Unit (ICU), decisions are needed regarding care. Here’s what patients need to know to choose the best rehab facility.
Freedom of Choice
“Although they may not know it, patients have considerable say about where they go following discharge from ICUs,” says Deniz Ozel, M.D., medical director, New England Rehabilitation Hospital, a world class rehabilitative hospital located in Woburn, Massachusetts. “Working with their case managers, they can become empowered and affect the decision-making process.”
Arthur Williams, M.D., medical director at Braintree Rehabilitation Hospital, another leading rehabilitative hospital in Braintree, Massachusetts, concurs. “Case managers are uniquely qualified to understand a patient’s diagnosis, insurance coverage, and make recommendations for a discharge plan,” says Williams. “It’s their job to find the right balance between medical care and rehabilitative therapy to help patients reach their goals and objectives.”
Typically, options include:
Skilled nursing facilities – offering less intensive rehabilitation therapy with management of non-complex medical issues;
Long term acute hospitals – offering management of multiple system failure with less focus on rehabilitation; and
Inpatient rehabilitative facilities – offering intensive rehabilitation services, with management of complex medical issues.
Inpatient rehabilitative facilities, dedicated to short-term rehabilitation, are ideal for those who have suffered a significant medical event, yet well enough to benefit from intensive therapy.
Patients with no prior rehab experience should network for recommendations. The case manager also should be able to refer local providers.
Top Criteria
With referrals in hand, here’s what to ask:
1. How will the facility help me reach my goals? Does it have success treating my type of injury? Look for a comprehensive plan of care. Ask about specialty programs for your condition.
2. How much therapy will I receive? Intensive programs offer a minimum of three hours of therapy a day, five days a week.
3. Who will provide my care? How often will I see a doctor or specialist? Ask who will comprise your team and if physician oversight is provided 24/7.
4. What technology is available that will benefit me? New devices incorporating functional electrical stimulation and robotics offer a track record of success.
5. How does the facility compare against the competition? Ask about accreditations like those from The Joint Commission, use of Functional Independence Measure (FIM) scores, and patient satisfaction surveys.
6. Check if the facility can improve functional outcomes in physical rehabilitation with the best and latest equipment to treat injured limbs and joints. If the Tutor system is used the center may be one of the best to choose from.
The newly developed HandTutor and its sister devices (ArmTutor, LegTutor, 3DTutor) have become a key system in neuromuscular rehabilitation and physical therapy for interactive rehabilitation exercise. These innovative devices implement an impairment based program with augmented feedback and encourage motor learning through intensive active exercises. These exercises are challenging and motivating and allow for repetitive training tailored to the patient’s performance. The system also includes objective quantitative evaluations that provide the therapist information to customize the most suitable rehabilitation program to the patient’s ability. Currently part of the rehabilitation program of leading U.S. and foreign hospitals the Tutors are also used in clinics and at home through the use of telerehabilitation.
Tuesday 18 October 2011
ArmTutor Compliments Stroke Therapy

Hema Vijay writing in THE HINDU on October 18, 2011 describes what Dr. Preeti Raghavan is involved in.
Dr. Raghavan holds a beacon of hope for those who have been incapacitated by stroke. Her study of memory and movement in the field of neuroscience has aided many to lead near normal lives
She teaches the brain to make new connections; connections which could help stroke victims regain the ability to move a finger, hand, leg or arm. Preeti Raghavan, MD, and the ‘brain’ behind the Motor Recovery Research Laboratory at the Rusk Institute of Rehabilitation Medicine, the premier rehabilitation hospital in New York State, believes in the awesome potential of the human body.
For many years now, Dr. Raghavan has been reverse engineering the neural pathway of movements. “Even if a part of the brain has been affected by stroke, the person can still relearn the movement — through an alternate pathway in the brain,” she says. Dr. Raghavan studied medicine at the Annamalai University and later at New York before going on to make path-breaking findings.
It all began when she started studying how people perform movements. Think of this; we never consciously calculate the amount of pressure or the extent of the turn we need to give our fingers to hold a spoon, open a tap or shake hands. “But actually, even a simple movement requires complex planning, which we learn and store in our memories for reuse,” Dr. Raghavan explains.
Four years ago, Dr. Raghavan was studying movement in stroke patients by using a simple grip device with sensors that measured forces produced by fingers when a movement is executed. “These people couldn’t work out the force required to grasp and lift the object. Their old memories had been erased by the stroke, and new memories were not allowed to be formed, because of the damage to the neurological tissue,” she recounts. It was then that Dr. Raghavan made the amazing discovery that, if the same people lift the object with the intact hand and then repeat the movement with the affected hand, the affected hand is able to learn to perform the movement! “The idea is to use alternate connections. Amazingly, our brains have developed many redundant neural pathways for the same function. We utilise those preserved parts of the brain to revoke the lost function,” Dr. Raghavan adds.
For instance, one of Dr. Raghavan’s patients was a young musician who had had a successful bone marrow treatment for cancer, and later had a stroke. He recovered from it enough to run marathons, but still couldn’t manage movements such as holding a toothbrush, or tying shoe laces. Now, with Dr. Raghavan’s strategies, this young man is ‘learning’ to do it!
“Advances in research such as in Dr. Raghavan’s lab are increasing the understanding of cerebral physiology and function needed to build the necessary framework for better treatments specific to individuals with unique injuries. The work in Dr. Raghavan’s lab is a great example of translating basic sciences into clinical practice — and is creating excitement in neuroscience advances,” says Steven Flanagan, MD, clinical professor and chairman, Department of Rehabilitation Medicine and medical director, Rusk Institute at NYU Langone Medical Center.
Dr. Raghavan also zeroed in on musicians as subjects of study, because, musicians happen to be among the most dexterous users of their limbs. This is how she discovered that professional pianists who activate their upper back muscles while playing the piano tend not to suffer from overuse strain or injuries, compared to those who use just their fingers and arms. “It is a popular misconception that muscles are just tissues for execution of action. But muscles are also important for our kinesthetic sense. That is how expert musicians know how to apply just enough force,” she remarks. She uses such insights to help stroke victims and others in regaining optimum use of their limbs. Dr. Raghavan is also studying how listening to music and patterning rehabilitation exercises alongside musical rhythms may enhance the speed of recovery tremendously. “Rhythm assists movement because, we move in space and time”, she says.
Working with her team of doctors, engineers, statisticians, physical and occupational therapists, Dr. Raghavan is helping stroke victims and others get movement back into their lives. Finally, some advice for all of us: “We are moving all day long. The hierarchy of movement has to be efficient; otherwise it can lead to trouble.”
In addition to Dr. Raghavan’s program the ArmTutor is a compliment to restoring normal movement to the patient’s upper extremities.
The ArmTutor™ system has been developed to allow for functional rehabilitation of the upper extremity. The system consists of an ergonomic wearable arm brace and dedicated rehabilitation software. The ArmTutor™ system allows for a range of biomechanical evaluation including speed, passive and active range of motion and motion analysis of the upper extremity. Quantitative biomechanical data allow for objective evaluation and rehabilitation treatment follow up. The ArmTutor™ rehabilitation concept is based on performing controlled exercise rehabilitation practice at a patient customized level with real time accurate feedback on the patient’s performance. The exercises are designed in the form of challenging games that are suitable for a wide variety of neurological and orthopedic injury and disease.
The games challenge the patient to perform the exercise task to their best ability and to continue exercise practice.
The ArmTutor™ allows for isolated and a combination of elbow and three directional shoulder treatment. The system provides detailed exercise performance instructions and precise feedback on the patients exercise performance. Controlled exercise of multijoints within the normal movement pattern prevents the development of undesired and compensatory joint movement and ensures better performance of functional tasks.
The ArmTutor™ system is used by many leading rehabilitation centers worldwide and has full FDA and CE certification.
Subscribe to:
Posts (Atom)